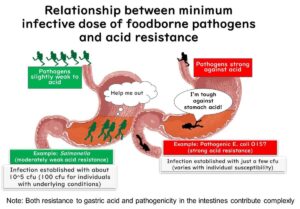
In this article, we'll explore the differing amounts of bacteria needed to cause food poisoning by two culprits: Salmonella and enterohemorrhagic Escherichia coli. Additionally, we'll discuss a major factor contributing to these differences: the varying resistance to stomach acid between the two.
Comparative Infectious Doses of Enterohemorrhagic E. coli and Salmonella
Infectious foodborne pathogens generally require ingestion through food to initiate infection. However, bacteria with high virulence can also transmit through other avenues such as surfaces or direct human contact. Enterohemorrhagic E. coli (EHEC) is an example of such a bacterium, while Salmonella typically does not spread through these non-food routes. What leads to this difference?
The differences in the infectious doses required to cause foodborne illnesses by these two bacteria are a significant factor.
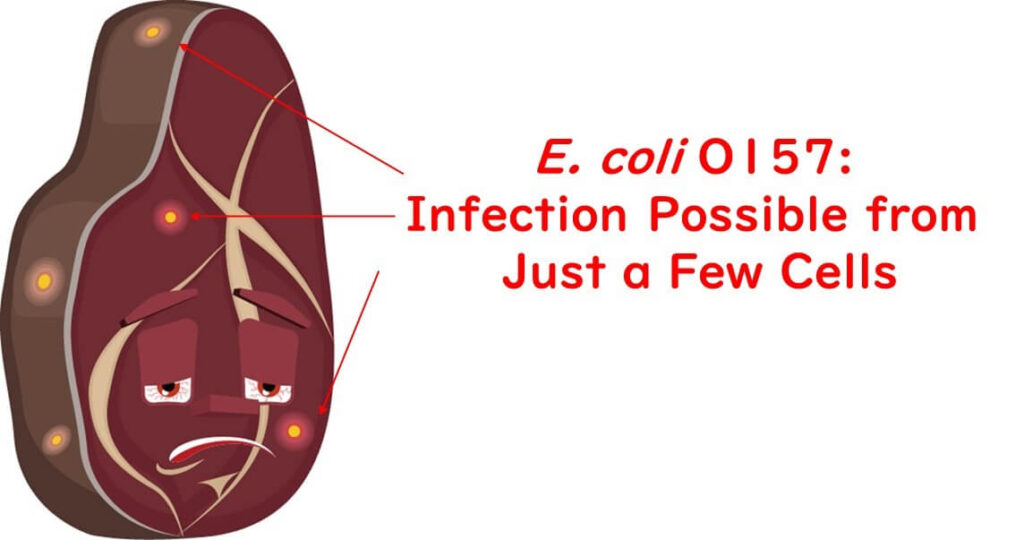
Enterohemorrhagic E. coli
There's a variety of data concerning the infectious dose of EHEC. According to the FAO and WHO (2011), some significant findings include:
- Based on retrospective analyses of food involved in outbreaks, the pathogen's ability to infect from person to person, and its resistance to acidic conditions in the stomach, the infectious dose of EHEC can be as few as several hundred cells, with some studies estimating as few as 10 ingested cells.
- Other studies have shown that even <2 cells per 25g of food can be sufficient to cause infection. Similar infectious dose estimates have been proposed by CAST (1994).
- For patients who consumed known quantities of contaminated dry fermented salami, retrospective calculations of the infectious dose ranged from 2 to 45 cfu.
- In a particular outbreak involving contaminated hamburger patties, the contamination per patty was between 0.9 to 4.3 cfu.
- Similarly, in another U.S. case, raw hamburger patties contained between 67 to 670 cfu per patty, suggesting an infectious dose under 700 cfu. It is reasonable to assume that cooked patties (at the time of consumption) contained fewer bacteria, although the exact number of bacteria ingested is unknown.
Overall, it seems reasonable to conclude that the infectious dose for EHEC could be in the order of a few cells.
Salmonella
For Salmonella, there are two types of estimates available: one from volunteer experiments and another from actual food poisoning cases (there are no volunteer experiment data for E. coli O157 due to its severe and dangerous symptoms).
- Volunteer experiments: Literature suggests that the infectious dose for various serogroups of Salmonella ranges from 10^5 to 10^10 cfu, with many textbooks indicating a typical infectious dose of about 10^5 cfu or more, based on these volunteer data(Kothry and Babu 2007).
- Estimates from actual food poisoning cases: Estimates based on real outbreak data suggest an infectious dose below 100 cfu (with 50% of people infected at a dose of 36 cfu), indicating that the infectious dose from real-world data tends to be lower than that estimated from volunteer experiments(Teunis et al., 2010).

As estimated from actual food poisoning incident data, the infectious dose turns out to be lower than that estimated from volunteer experiments.
The main reason for this difference in estimated values might be attributed to the following:
- The components of the food involved in the outbreaks could be playing a protective role against stomach acid. Most volunteer experiments involve directly ingesting the bacteria without any food-based protection, thus exposing the bacteria to harsh conditions where they are more likely to be killed by stomach acid.
- Individuals who tend to become patients in actual outbreaks, such as infants, the elderly, and those with underlying health conditions, are more susceptible to Salmonella infection compared to healthy adults who are generally used in volunteer experiments.
Thus, despite the uncertainty surrounding the exact infectious doses, considering these factors, it's reasonable to conclude that the infectious dose for Salmonella is generally higher compared to that for enterohemorrhagic E. coli.
Resistance of Salmonella and Enterohemorrhagic E. coli to Acid
The differences in the infectious doses of foodborne pathogens are influenced by various factors including their resistance to stomach acid, resistance to bile acids secreted in the small intestine, competitiveness with the gut microbiota, and the ability to evade immune cells in the intestinal epithelial cells. However, among these factors, the most significant is believed to be the resistance to stomach acid, which is the first step.
Below, I will introduce some studies that directly compare the acid resistance of Salmonella and enterohemorrhagic Escherichia coli.
Experiments in Liquid Media
Firstly, let's discuss a study that examined the survival of E. coli O157:H7 and Salmonella in tryptic soy broth (TSB) adjusted to a pH of 3.5 at 30°C.
Note that while the paper also includes experiments on Listeria, those are omitted here. Additionally, experiments on the effects of prior adaptation to acid are also excluded from this article.
- In the study, Salmonella showed a significant reduction in bacterial count, dropping by over seven digits within 2 hours in TSB at pH 3.5.
- In contrast, E. coli O157:H7 exhibited a smaller reduction in count, with only a three-digit decrease even after 8 hours.
These findings indicate that E. coli O157 has a higher resistance to acid in liquid media compared to Salmonella.
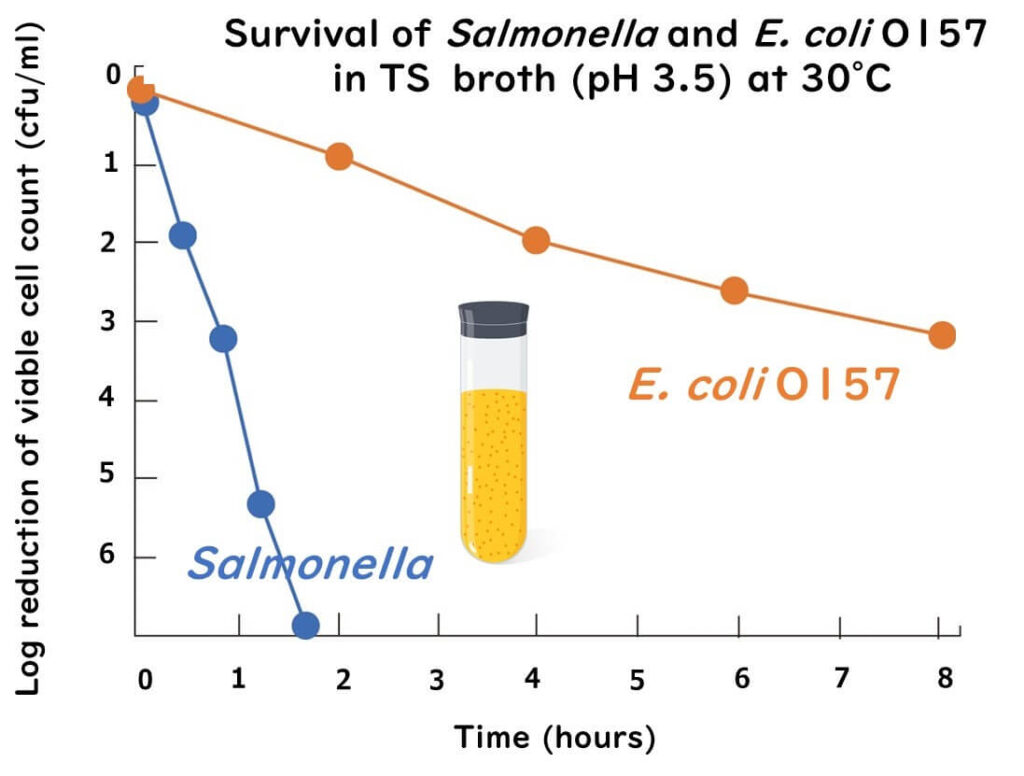
The figure above is drawn from data in the following paper.
Comparative acid stress response of Listeria monocytogenes, E. coli O157:H7 and Salmonella Typhimurium after habituation at different pH conditions
Letters in Applied Microbiology, 38, 321-326 (2004)
Experiments with Food
Next, I'll introduce a study that used beef homogenate to investigate the survival of enterohemorrhagic E. coli O157 (STEC) and Salmonella. After inoculating a sterile 10% beef homogenate, 5% lactic acid was added, and their survival was assessed.
Note that this paper also compares the acid resistance of wild-type strains to antibiotic-resistant strains, but these details are omitted here.
- Of the Salmonella strains tested, 87.9% (29 out of 33 isolates) reached the detection limit within 0 to 4 minutes.
- In contrast, E. coli O157:H7 took up to 8 minutes to decrease to the detection limit.
These results suggest that Salmonella has weaker resistance to acid when lactic acid is used compared to E. coli O157:H7.
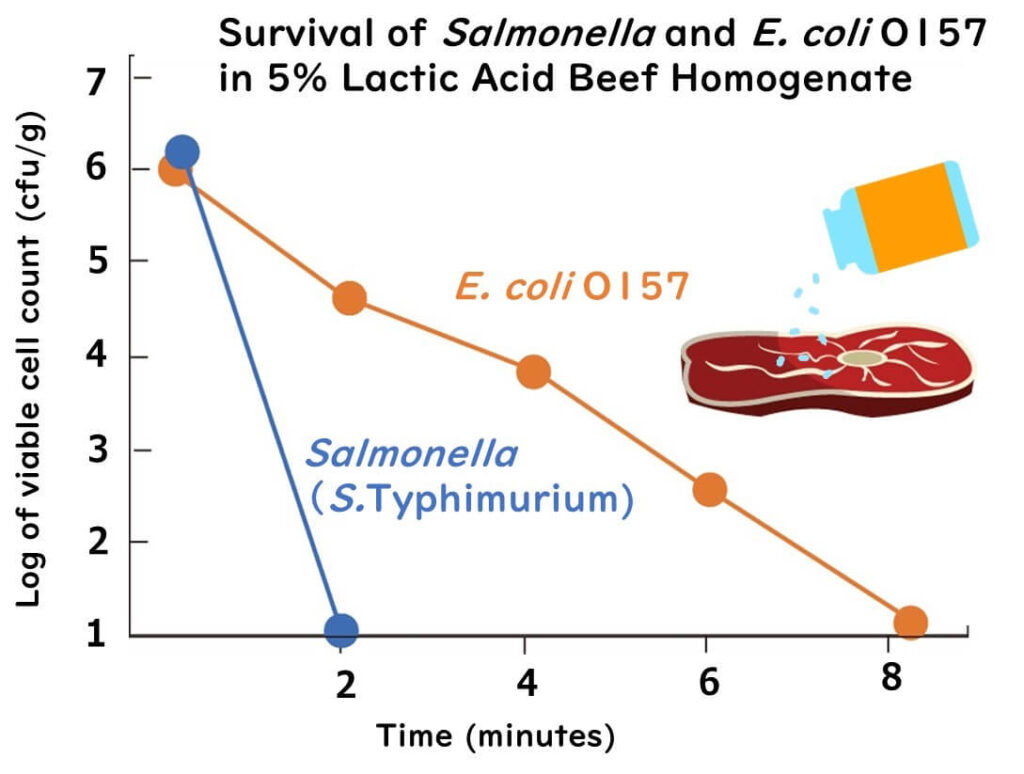
The figure above is drawn from data in the following paper.
Lactic acid resistance of Shiga toxin-producing E. coli and multidrug-resistant and susceptible Salmonella Typhimurium and Salmonella Newport in meat homogenate
Food Microbiology, 36, 260-266(2013)
Experiments with Stomach Acid
So, how do these two bacteria fare in an environment simulating the human stomach? I'll present a study comparing the survival of E. coli O157 and Salmonella in simulated gastric acid.
Note that this paper also involves experiments on Listeria, which are omitted here. Moreover, it includes survival experiments in unpasteurized, preservative-free apple cider at low temperatures (pH 3.3-3.5), which are also excluded from this article.
- In the experiments, Salmonella exhibited a decrease of over six digits within 5 minutes.
- E. coli O157 showed only a modest decrease, around two digits, even after 180 minutes.
From these results, it is clear that E. coli O157 is more resistant to stomach acid compared to Salmonella.
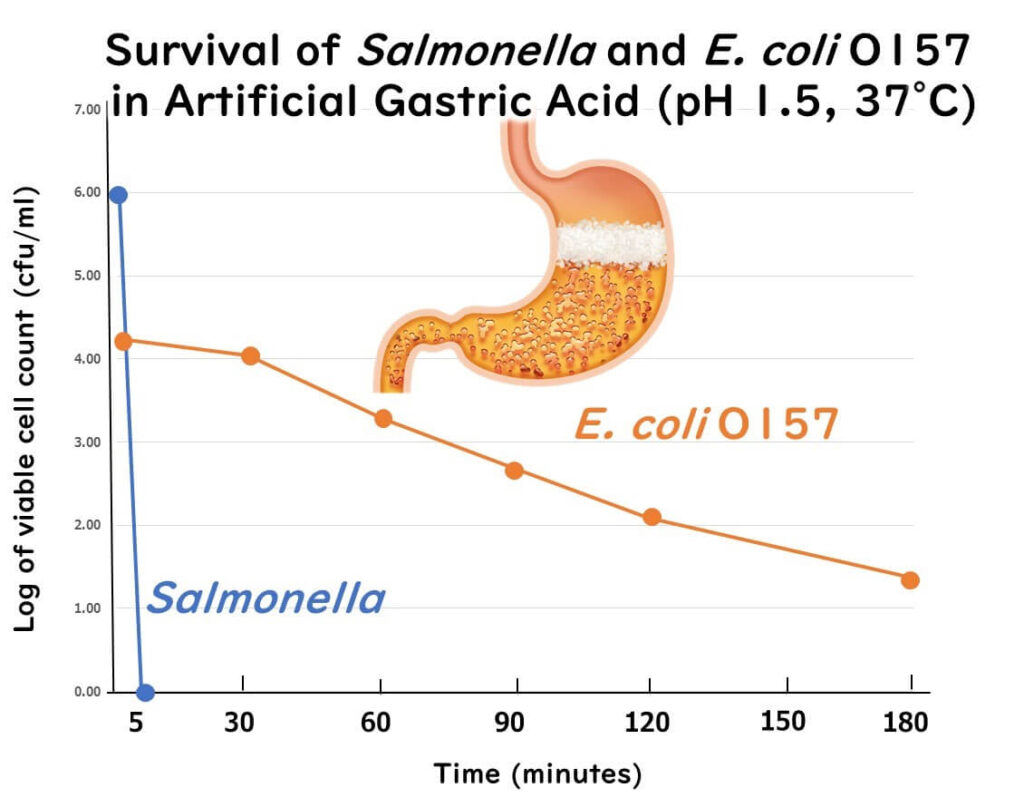
The figure above is drawn from data in the following paper.
Comparative survival of Salmonella typhimurium DT 104, Listeria monocytogenes, and E. coli O157:H7 in preservative-free apple cider and simulated gastric fluid.
International Journal of Food Microbiology 46 (1999) 263–269
Overall, enterohemorrhagic E. coli demonstrates stronger resistance to various acids, including stomach acid, than Salmonella. The mechanisms behind the strong acid resistance of enterohemorrhagic E. coli are not yet fully understood.
As for the mechanisms of acid resistance in bacteria, several amino acid decarboxylases have been identified. Decarboxylases such as glutamate, arginine, and lysine decarboxylase work by incorporating their target amino acids into the cell, where they undergo decarboxylation, consuming one H+ ion in the process. This helps to alkalize the cytoplasm during amino acid decarboxylation, thereby protecting the bacterial cell. Among these, the glutamate decarboxylase (GAD) used by enterohemorrhagic E. coli is considered one of the most potent acid resistance mechanisms (Diez0Gonzalez and Karaibrahimoglu 2004).
Summary
As we've discussed, the differences in the infectious doses and resistance to stomach acid between Salmonella and enterohemorrhagic E. coli significantly impact the infectious doses required for these two foodborne pathogens to cause illness.
However, the reason why enterohemorrhagic E. coli has such a low infectious dose is not only due to its relatively strong resistance to stomach acid but also because of its potent pathogenicity. The toxin it produces on the intestinal epithelial cells, known as Shiga toxin, is so powerful that even a small number of cells can cause significant damage to the intestinal wall. This toxin has lethal effects on vascular endothelial cells even in minuscule amounts, leading to severe disease. Therefore, infections caused by enterohemorrhagic E. coli are likely to occur due to a combination of resistance to stomach acid and strong pathogenicity.