Salmonella is a bacterium known for causing food poisoning worldwide, but it also has more severe strains that can lead to life-threatening infections. In this article, we explore Salmonella's characteristics, from its habitats and survival traits to its types—those responsible for food poisoning and those that spread through person-to-person transmission. We'll also cover critical aspects of Salmonella's serotype notation, contamination in raw chicken, the latest global regulations, risks associated with eggs, and its unique resilience to drying. Whether you're a food industry professional or a curious reader, this guide provides valuable insights into preventing and managing Salmonella-related risks.
Unraveling the Domino Traits of Salmonella: A Journey from Habitat to Characteristics
Before we delve into this sequence of traits, it would be helpful to read our foundational article on Gram staining and microbial characteristics available on our blog. This background reading will make understanding the characteristics of Salmonella smoother, much like the fall of aligned dominos.
Gram Staining and Microbial Properties: A Comprehensive Overview
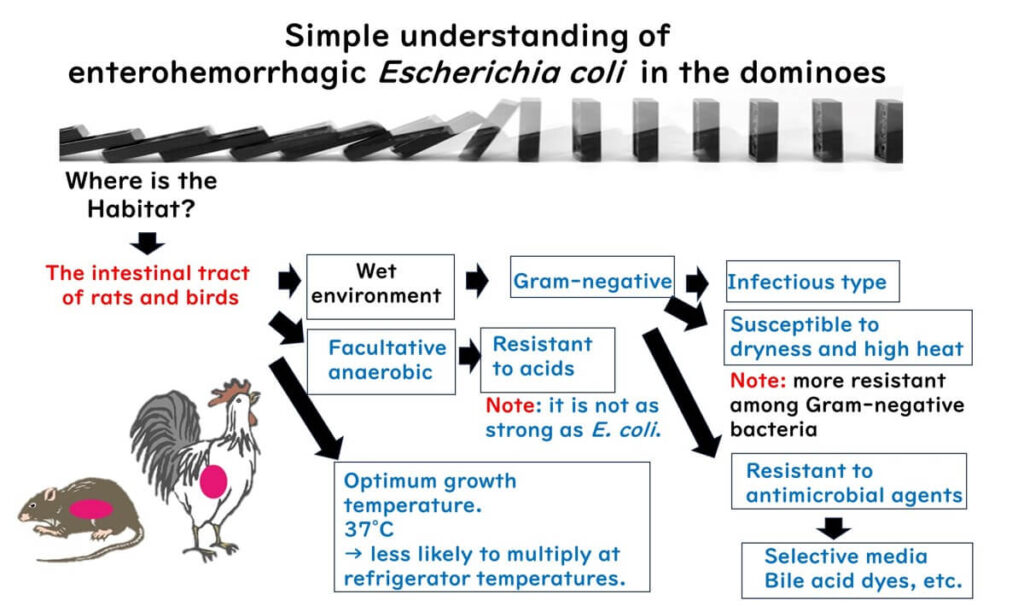
- Habitat in Watery Environments: The journey of understanding Salmonella begins with its habitat in the intestines of rodents and poultry, which are typically moist environments.
- Gram-negative Bacteria: Given this habitat, Salmonella is classified as a Gram-negative bacterium.
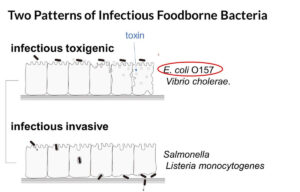
- Cause of Infectious Food Poisoning: The Gram-negative structure of Salmonella enables it to cause infectious food poisoning, a significant concern in food safety.
- Temperature Preference: Salmonella multiplies optimally around 37°C, close to the body temperature of mammals and birds, meaning it does not thrive in colder settings like refrigerators.
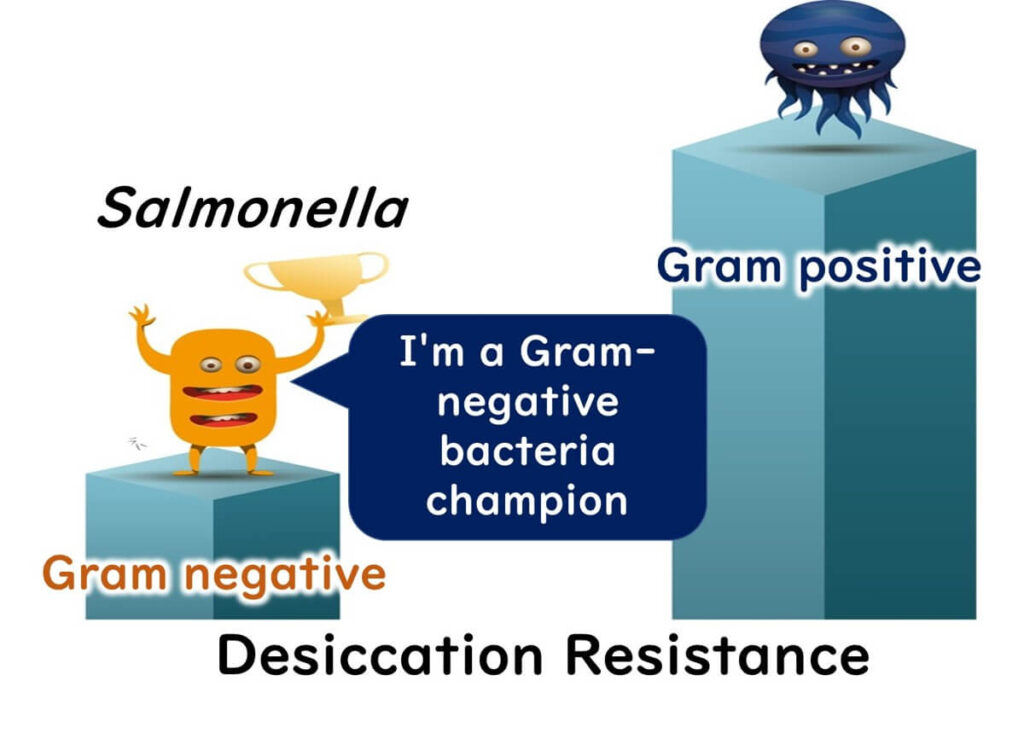
- Resistance to Drying: Despite its Gram-negative classification, Salmonella shows remarkable resistance to dry conditions compared to other Gram-negative bacteria. This resilience is crucial in food safety, as Salmonella can survive on relatively dry manufacturing lines or in dry food products.
- Facultative Anaerobes: Adapted to life in the intestines, Salmonella is facultatively anaerobic, allowing it to survive and grow in both low and high oxygen environments.
- Organic Acid Production: Like other intestinal bacteria, Salmonella can produce organic acids through fermentation, giving it some resilience to acidic conditions, though not as robust as that of E. coli.
- Protective Outer Membrane: The Gram-negative outer membrane of Salmonella provides a strong defense against hydrophobic compounds, aiding its survival.
- Selective Growth in Media: This protective membrane allows selective media to be designed for isolating Salmonella, by adding specific compounds that inhibit Gram-positive bacteria, making Salmonella easier to identify and study.
Understanding these traits in sequence, much like the toppling of dominos, provides a clear view of Salmonella’s characteristics and highlights the necessary precautions to prevent foodborne illnesses.
The Dual Nature of Salmonella: A Tale of Two Types
When we discuss Salmonella, it’s essential to recognize that we are broadly referring to two distinct types of pathogens.
Food Poisoning Culprits
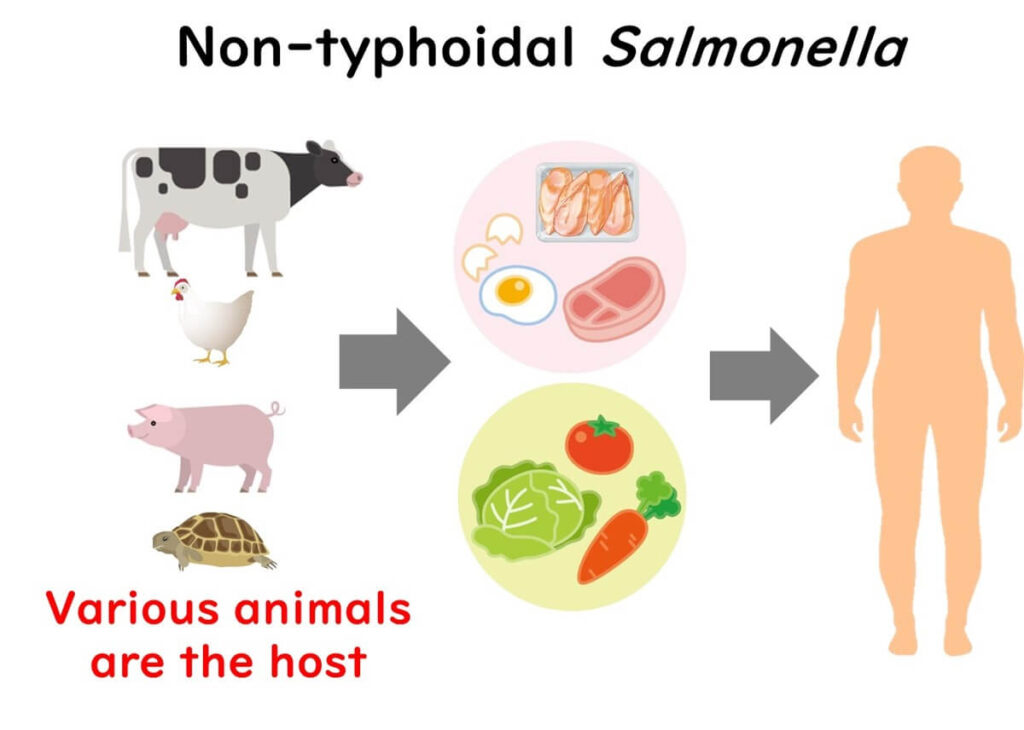
The first type of Salmonella, including strains like Salmonella Typhimurium and Salmonella Enteritidis, causes the common form of food poisoning. These strains typically enter the body through contaminated food. Originating from sources such as birds, rodents, and other warm-blooded animals, these strains are widespread causes of food poisoning, especially in developed countries. Thorough cooking and proper food storage are essential to prevent these kinds of infections.
Typhoid and Paratyphoid Infections
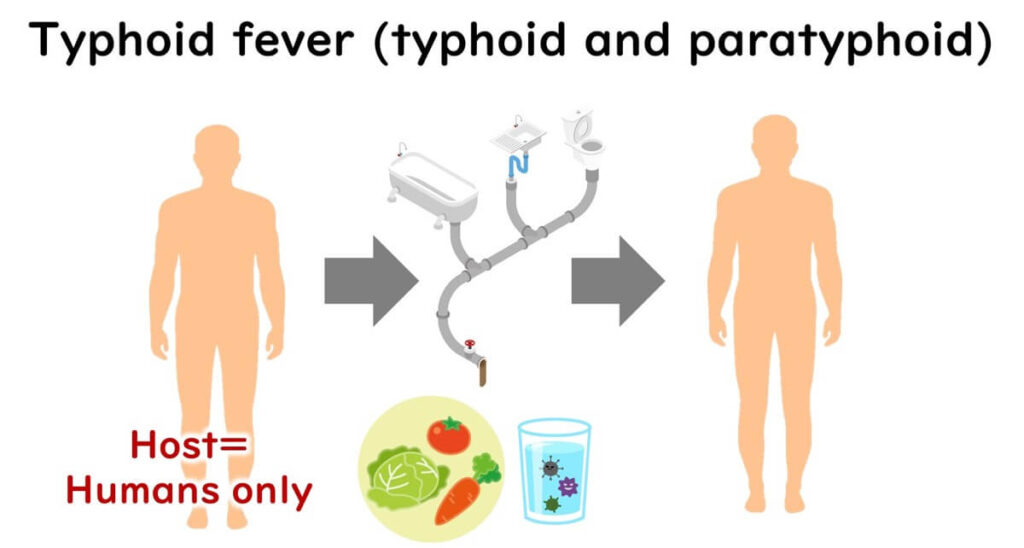
The second, more dangerous type includes strains such as Salmonella Typhi, responsible for Typhoid fever, and Salmonella Paratyphi A, which causes Paratyphoid fever. These strains primarily infect humans and are classified as infectious diseases due to their ability to enter the bloodstream, posing a higher risk of severe illness and mortality. Controlling food hygiene is vital to managing these infections, especially in developing countries where limited water and sanitation facilities can increase the risk of transmission. Travelers from developed countries should be cautious when visiting areas where these infections are more common.
Distinct Invasion Mechanisms
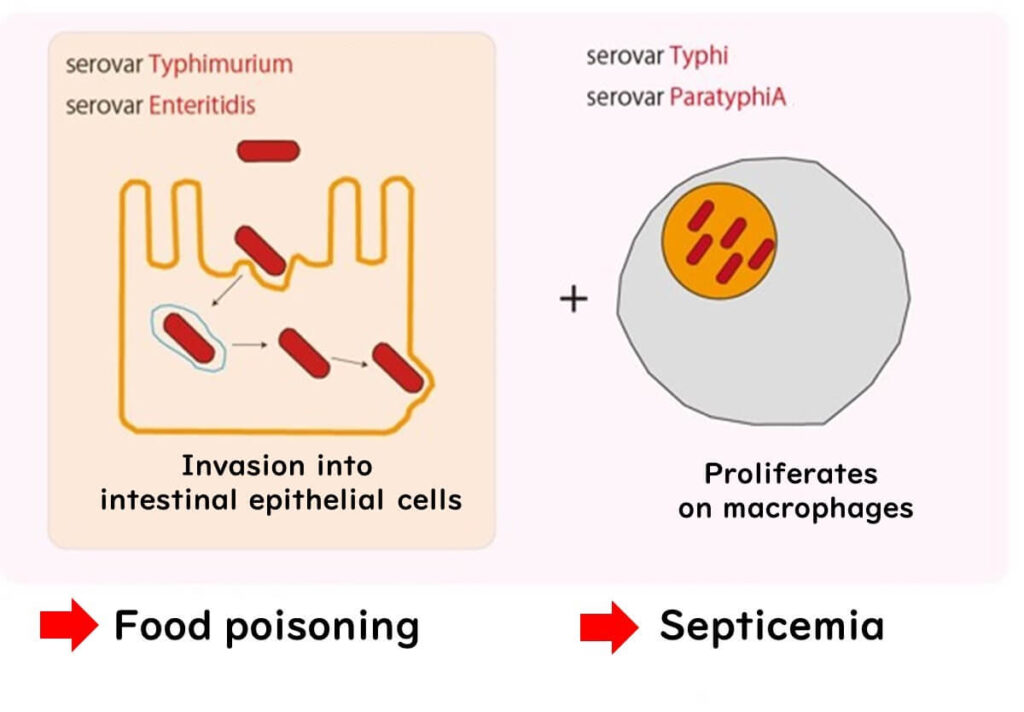
Both groups operate differently once they enter our system. The food poisoning strains, like Salmonella Typhimurium and Salmonella Enteritidis, invade the intestinal cells but are eventually eradicated by the immune cells known as phagocytes. In contrast, Salmonella Typhi and Salmonella Paratyphi A possess an advanced mechanism to evade digestion by phagocytes, enabling them to spread via the bloodstream. This evasion results in more severe systemic symptoms and an increased mortality risk.
Understanding the dual nature of Salmonella gives us valuable insights into its diverse infection strategies. This knowledge is essential for implementing better health and food safety practices.
The Unique Notation of Salmonella: Denoted by Serotype
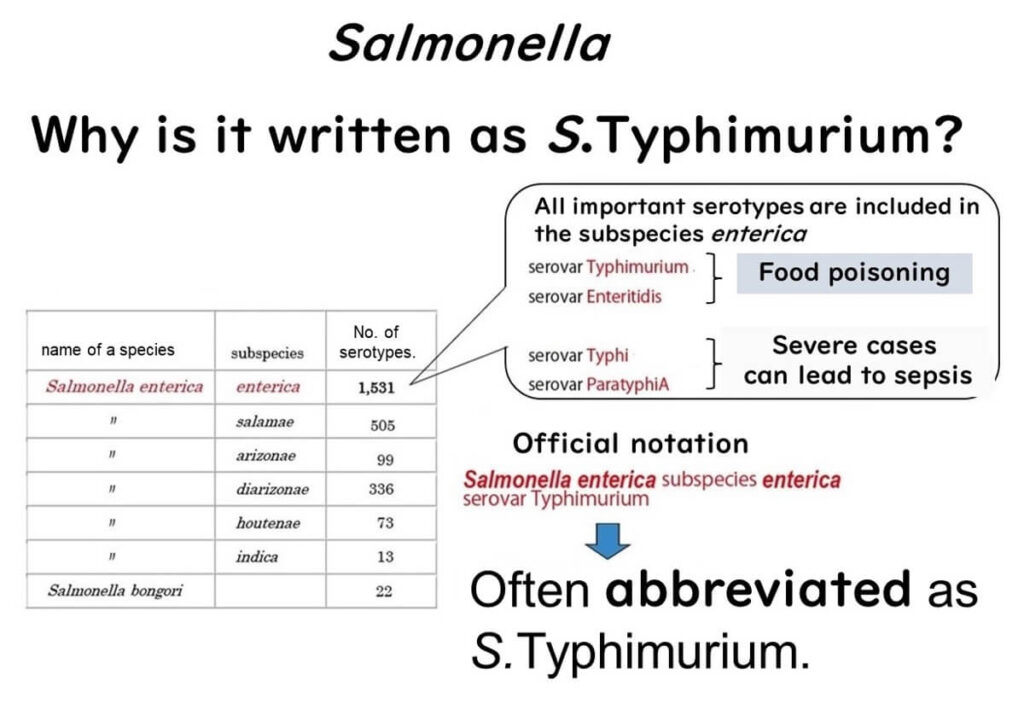
The notation of Salmonella differs slightly from how most bacteria are commonly written. Typically, bacterial names are italicized, with the species name beginning in lowercase (e.g., Staphylococcus aureus and Escherichia coli). However, Salmonella serotypes are an exception. For instance, the name “Typhimurium” starts with an uppercase "T" and is not italicized. Why the unique formatting?
Classification by Species and Subspecies
All strains relevant to food microbiology fall under the species Salmonella enterica, specifically the subspecies enterica, which includes strains responsible for foodborne illness, Typhoid, and Paratyphoid fevers. This species and subspecies classification would technically require a long name: Salmonella enterica subspecies enterica serovar Typhimurium.
Simplified Naming for Practicality
Writing out the full name each time is cumbersome. Thus, in academic and scientific contexts, it has become common to abbreviate and simply refer to the serotype, such as Typhimurium, written in block letters with an uppercase "T." While not an official convention, this shorthand is widely accepted for convenience.
Ease of Communication
This naming method helps clearly distinguish between strains and is a practical adaptation in scientific literature, especially when addressing specific serotypes associated with different types of illnesses.
This unique notation for Salmonella serotypes reflects a balance between scientific precision and practical communication, enabling clearer differentiation among strains without lengthy formal names.
Patterns of Salmonella Food Poisoning
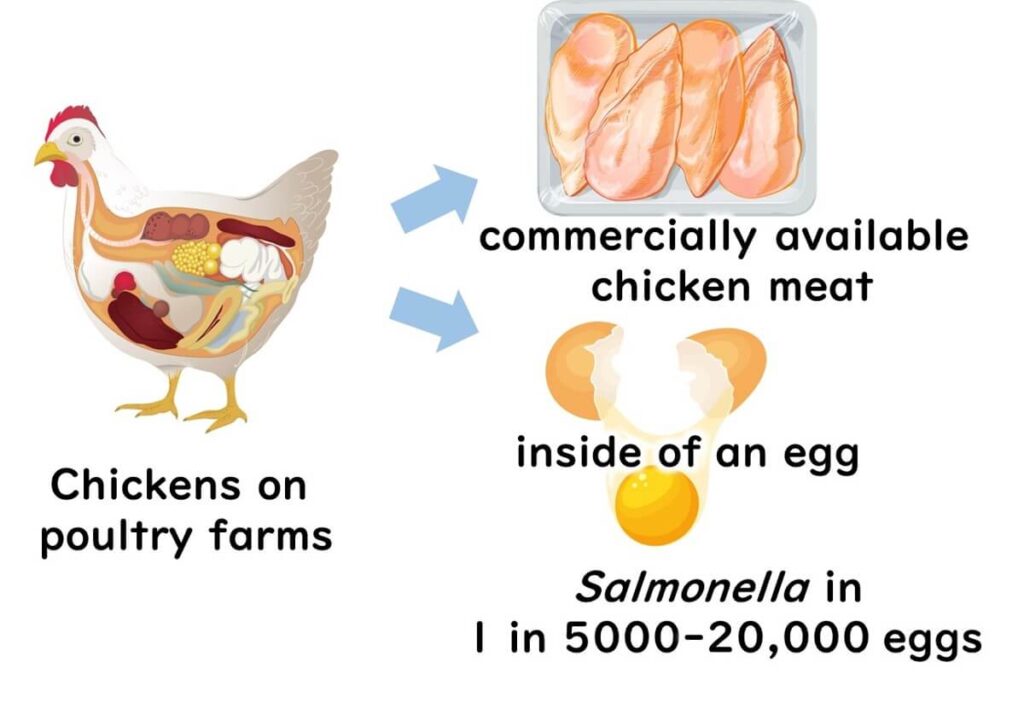
Salmonella is well-known for causing food poisoning, with chicken products being particularly high-risk due to the bacteria's frequent presence in poultry. It's common to detect Salmonella in chicken or other meats during routine inspections. Fortunately, thorough cooking effectively eliminates these bacteria, rendering the meat safe for consumption.
There are also instances of contamination in eggs through vertical transmission from parent chickens. It's estimated that globally, contamination rates for raw eggs vary between 1 in 5,000 to 1 in 20,000 eggs. Notably, the initial level of Salmonella present at the time the egg is laid generally remains stable throughout distribution.
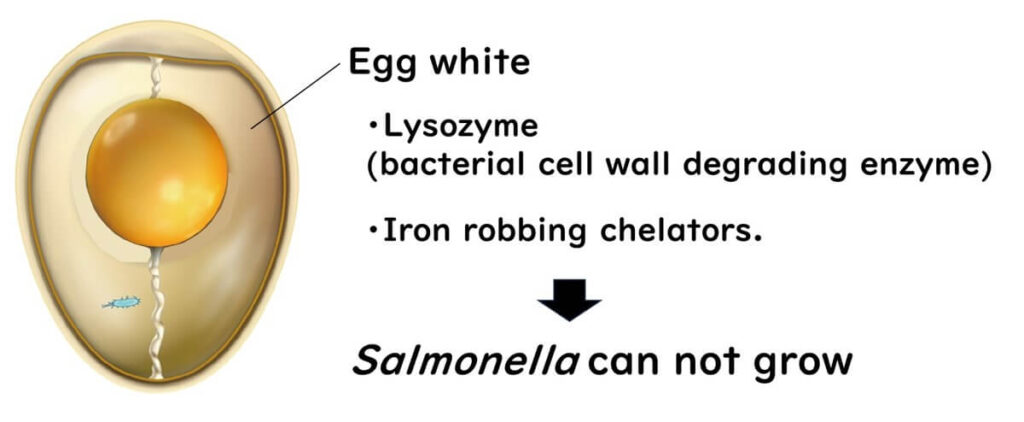
Why does Salmonella not multiply significantly within the egg during distribution? The answer lies in the egg white, which contains natural antibacterial substances. These include lysozyme, an enzyme that dissolves bacterial cell walls, and compounds that chelate iron—a nutrient essential for bacterial growth. These protective factors make it difficult for Salmonella to proliferate, even if contamination occurs.
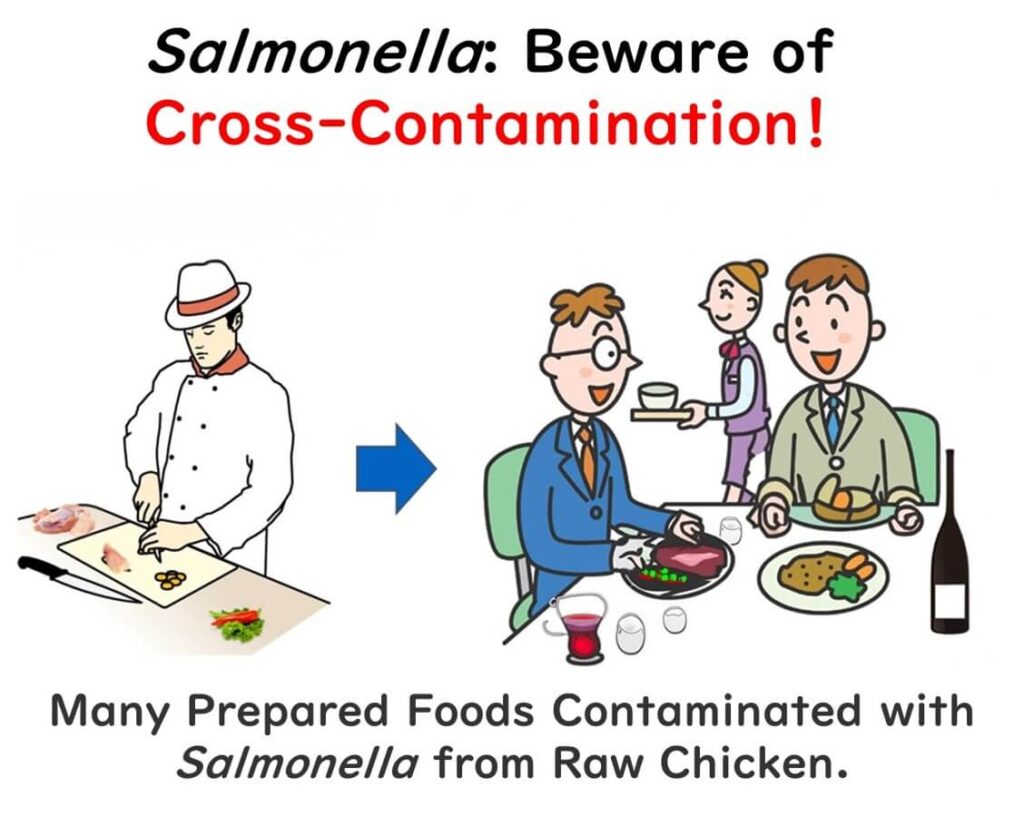
However, cross-contamination poses a risk. For instance, using the same knife or cutting board for both raw chicken and ready-to-eat foods like salad can transfer Salmonella from the meat to fresh ingredients. This is why kitchen hygiene practices, such as washing utensils and cutting boards after handling raw meat and thoroughly cooking poultry, are crucial in preventing Salmonella food poisoning.
Salmonella Contamination in Raw Chicken Meat
Salmonella contamination is a significant concern in raw chicken meat, with the bacterium commonly found in poultry. Understanding how this contamination is managed internationally helps us gauge food safety standards. Below, we explore the EU and US approaches to handling Salmonella in poultry.
The EU's Strict Regulations on Raw Chicken Meat
The European Union (EU) has established stringent standards for microbial contamination in poultry. Since December 2011, the EU requires that Salmonella Enteritidis and Salmonella Typhimurium must not be detected in 25 grams of chicken meat, based on a sampling size of five (n=5). This shift, from no specific microbial standards prior to 2010 to rigorous standards, demonstrates the EU's commitment to reducing foodborne illness.

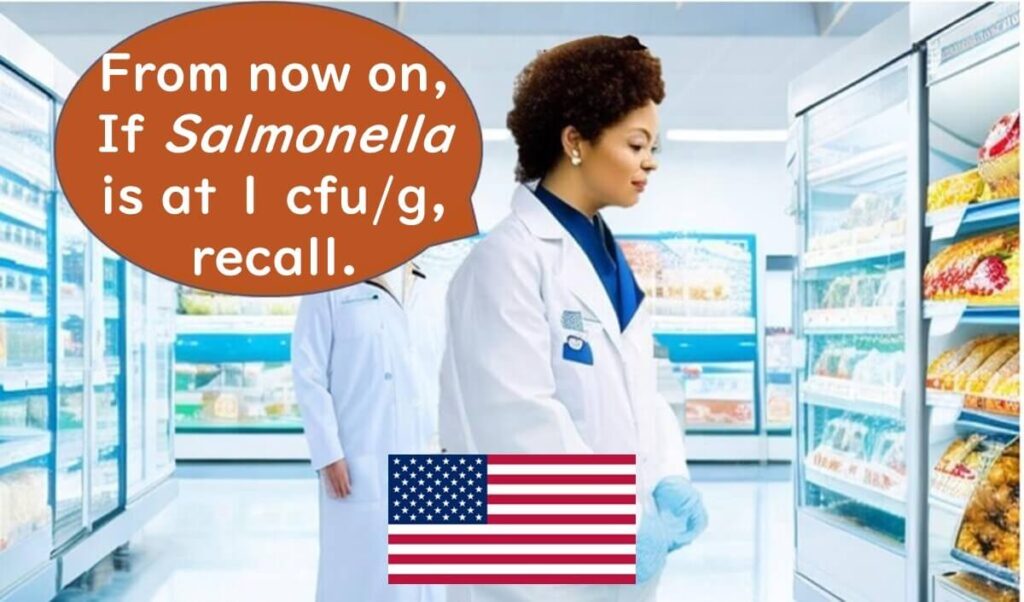
The US Initiates Regulations on Raw Chicken Meat
In the United States, the USDA has implemented standards targeting Salmonella in breaded raw chicken products as of April 2023. These standards, originating from policies announced in August 2022, mandate that products with more than 1 CFU/g of Salmonella prior to stuffing or breading cannot be sold. Should contamination be detected, affected products must be recalled, underscoring the USDA’s emphasis on food safety.
The push for eliminating Salmonella contamination in raw chicken presents a notable challenge for the industry. While Japan currently lacks specific microbial standards for raw chicken meat, the developments in the EU and US suggest that similar standards may soon be considered.
Understanding and adhering to these international standards not only highlights the importance of food safety but also helps to mitigate the risks associated with consuming raw or undercooked poultry.
The Scary Side of Cracked Eggs
When an egg is cracked, and the yolk mixes with the white, the risk of Salmonella contamination increases significantly compared to consuming the egg whole. The yolk is rich in nutrients, including iron, which Salmonella needs to grow. Once an egg is broken, Salmonella, if present, begins to multiply quickly in the mixture of yolk and white.
This is why many cases of Salmonella food poisoning are linked to dishes made from cracked eggs, like omelettes, scrambled eggs, cheesecakes, or homemade mayonnaise. Often, these cases arise due to improper handling of cracked eggs, such as insufficient sterilization or lack of temperature control.
If Salmonella contamination is on the eggshell, cross-contamination can easily occur. Therefore, careful egg handling and hygiene are essential when preparing foods that use raw or lightly cooked eggs.

How Resistant is Salmonella to Drying?
Interestingly, Salmonella demonstrates a notable resistance to drying, especially compared to other Gram-negative bacteria. For example, in Japan, a Salmonella outbreak was linked to dried squid snacks in 1999, highlighting how resilient it can be even in low-moisture foods.
In the U.S., Salmonella contamination incidents have been reported with peanut butter, a product with a low water activity of around 0.35, illustrating the bacterium's ability to survive in dry conditions.
In Europe, Salmonella has also been linked to contamination in chocolate products, highlighting that this pathogen can pose risks in low-moisture foods across different types of dry environments.

To illustrate this resistance further, an experiment compared Staphylococcus aureus (a Gram-positive bacterium) with Salmonella and Campylobacter, both Gram-negative. Campylobacter was the most sensitive to drying, while Salmonella showed significantly higher resistance than Campylobacter but still less than Staphylococcus aureus.
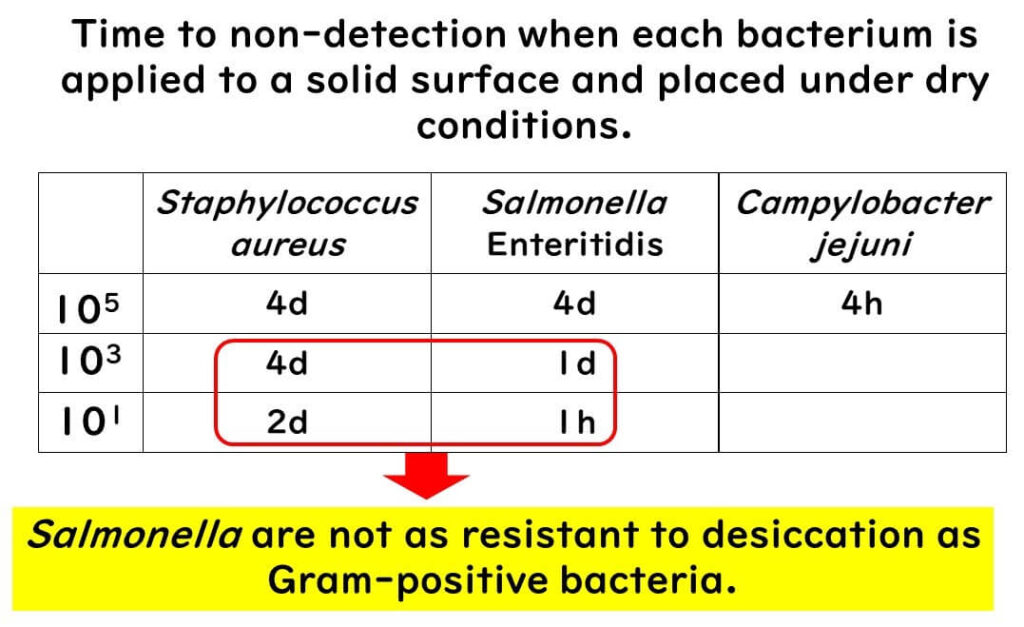
While Salmonella is more resilient to drying among Gram-negative bacteria, it does not reach the durability of Gram-positive types like Staphylococcus aureus. This difference underscores the importance of understanding the drying tolerance of pathogens to manage food safety effectively.