Staphylococcus aureus is a bacterium that walks a fine line between being a harmless resident of mammalian skin and a dangerous cause of foodborne illnesses. In this guide, we explore its habitats, how it produces heat-resistant enterotoxins, and its dual role as an opportunistic pathogen. Whether you're a microbiology enthusiast or a food safety manager, this post will provide you with practical insights into managing the risks associated with S. aureus.
Understanding Staphylococcus aureus: A Domino Effect from its Habitat
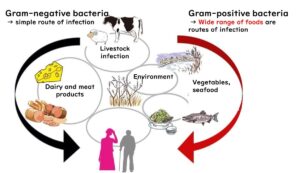
To fully appreciate the fascinating biology of Staphylococcus aureus, let’s first build a solid foundation. If you’re new to concepts like Gram staining and microbial characteristics, we recommend starting with our introductory article on these topics. It’s a great primer to set the stage for what’s to come.
Gram Staining and Microbial Properties: A Comprehensive Overview
The Domino Effect of Microbial Understanding
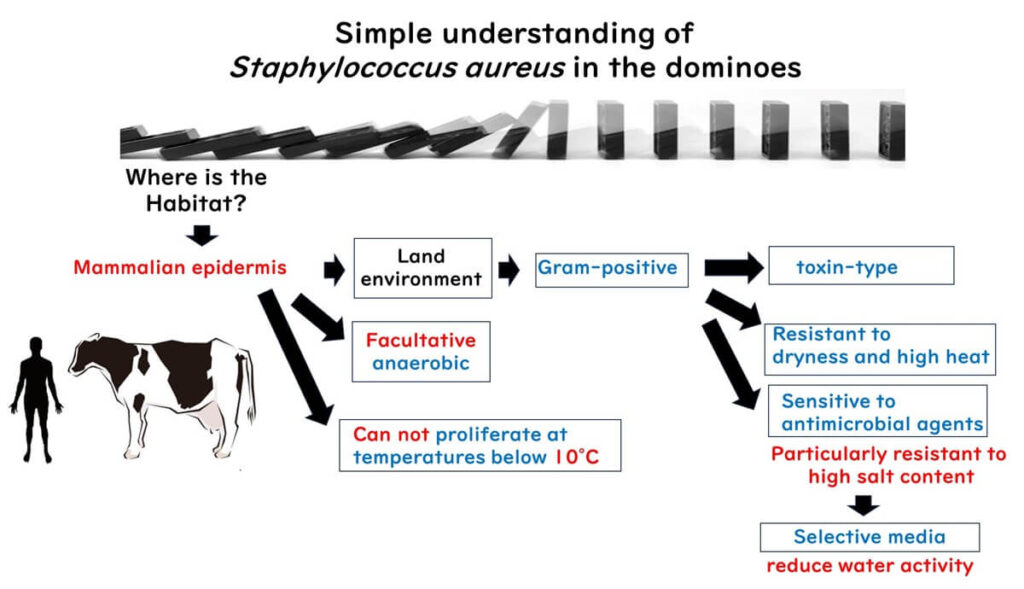
Let’s dive into Staphylococcus aureus, a bacterium that’s both intriguing and notorious. Imagine its key traits unfolding like a series of dominoes, each revealing an aspect of its nature:
Where Does It Live?
Staphylococcus aureus thrives on mammalian skin, where it resides as a harmless squatter in most cases.
Gram-Positive Identity
Its Gram-positive nature reflects its adaptation to the terrestrial environment of mammalian skin. This tough cell wall makes it resilient to physical stress.
A Food Poisoning Culprit
As a Gram-positive bacterium, it’s closely associated with toxin-related food poisoning – not the kind of guest you want at the dinner table.
Cold Intolerance
Unlike some bacteria, Staphylococcus aureus struggles in fridge-like temperatures. It thrives at 37°C, the temperature of the human body, making refrigeration an effective deterrent.
Resilient to Stress
S. aureus can withstand dryness and heat, living up to its reputation as a bacterial survivalist.
Low Oxygen? No Problem!
While some skin bacteria, like Micrococcus, require oxygen, S. aureus can thrive in oxygen-deprived zones, showcasing its versatility as a facultative anaerobe.
Acidic Conditions
By secreting organic acids, it creates environments that are favorable to its survival, even in acidic conditions.
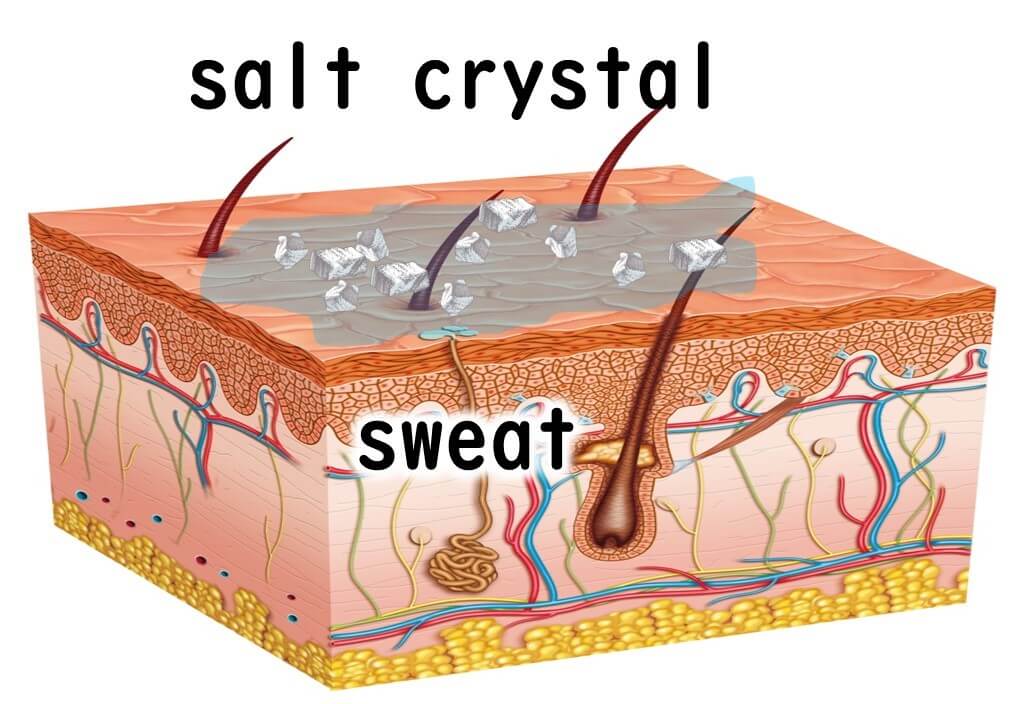
Salt Tolerance as a Survival Mechanism
S. aureus has adapted to salty environments, such as dried sweat on skin. This trait is exploited in selective media like Mannitol Salt Agar, where high salt concentrations inhibit other microbes.
A Chain Reaction of Understanding
By viewing these traits as interconnected pieces, Staphylococcus aureus becomes less of a mystery. Its survival strategies and risks in food safety make it an essential subject for anyone interested in microbiology or public health.
Staphylococcus aureus - A Opportunistic Infection Agent on Skin
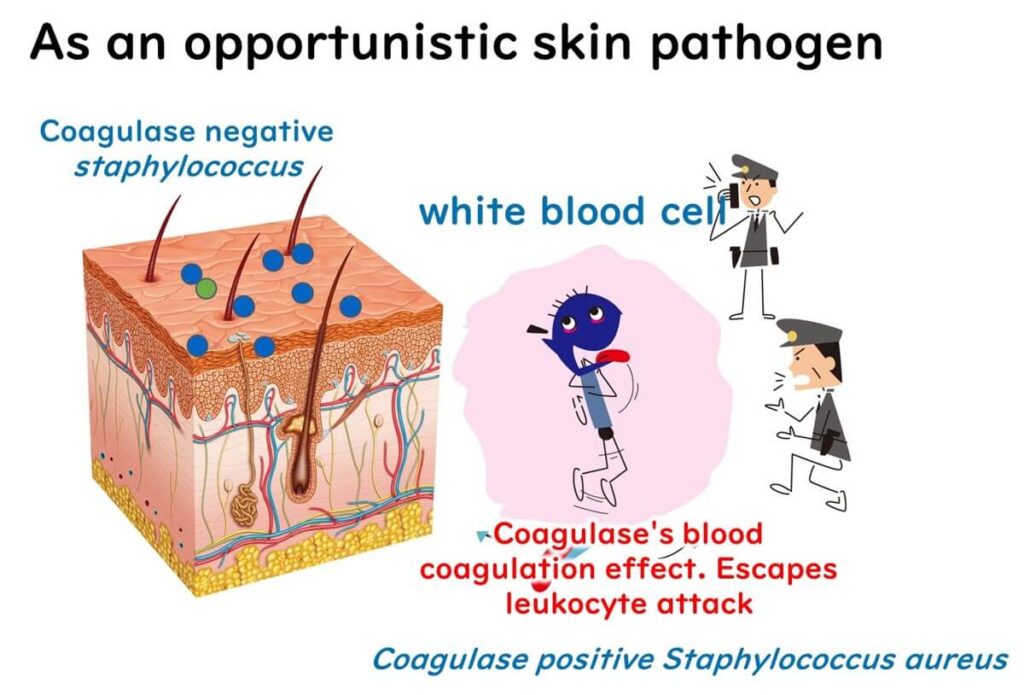
Staphylococcus aureus is a Gram-positive bacterium that freeloads on the skin of mammals. You'll find these tiny squatters living on the surface of our hands and inside our noses, feasting on the nutrients in our sweat. They're generally harmless, but when our body is under the weather and our immune system takes a hit, these bacteria seize the moment to invade our bodies. This type of bacteria, which takes advantage of weakened immune systems, is known as an opportunistic pathogen. It's like that sneaky friend who only shows up when there's pizza. Staphylococcus aureus often causes trouble in cases of acne, chapped hands, and skin inflammation in atopic dermatitis.
Role of coagulase during skin infection
Not all skin bacteria belong to Staphylococcus aureus. Within the Staphylococcus genus alone, there are over 30 types of Gram-positive cocci. What sets S. aureus apart is its ability to produce coagulase, an enzyme that clots blood plasma. By doing so, the bacterium builds a protective barrier of clotted blood around itself, shielding it from white blood cells. This strategy is like constructing a fortified wall – a survival mechanism that makes it harder for the immune system to eliminate the invader.
The Role of Enterotoxins During Opportunistic Skin Infections
Enterotoxins produced by S. aureus play a critical role in skin infections as superantigens, which disrupt the body’s immune response.
What is a Superantigen?
To understand superantigens, let’s briefly review the immune response:
- When bacteria invade the body, immune cells called macrophages engulf the bacteria and display fragments (antigens) to T-cells, the immune cells responsible for creating targeted antibodies.
- Normally, this antigen presentation is highly specific, like a lock and key mechanism, ensuring a precise immune response.
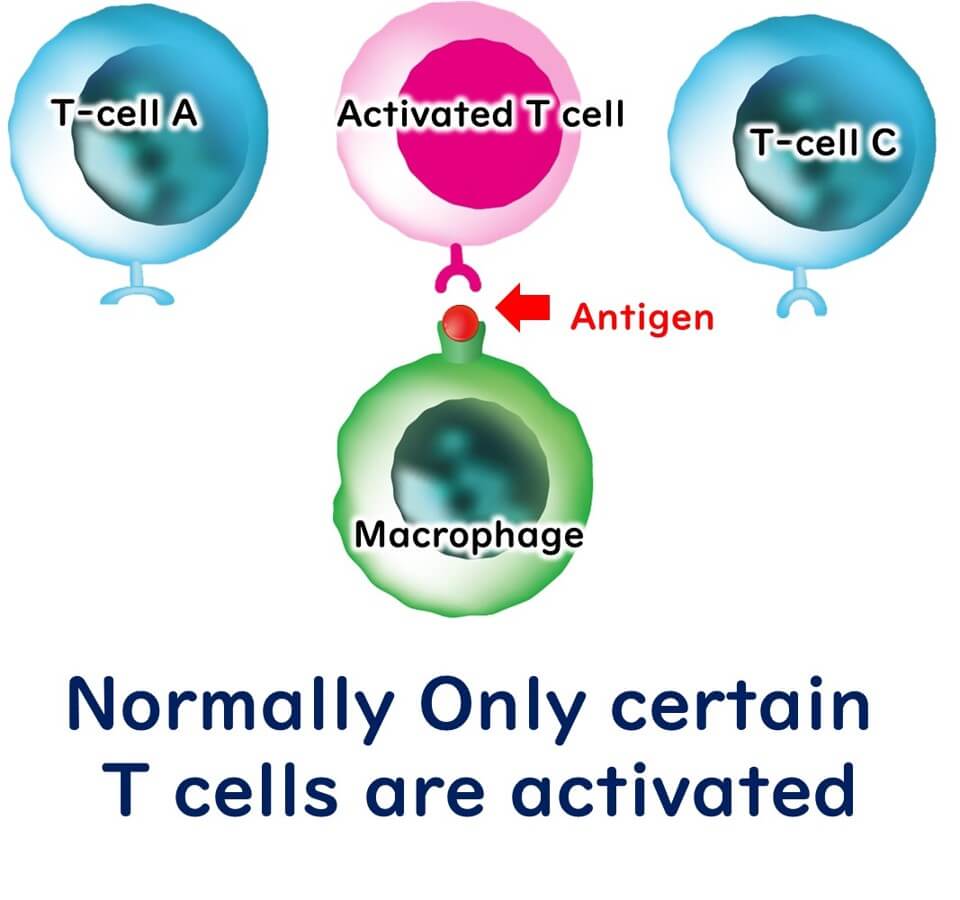
Superantigens, however, bypass this specificity. They bind simultaneously to antigen-presenting cells and T-cells, activating a large, non-specific number of T-cells.
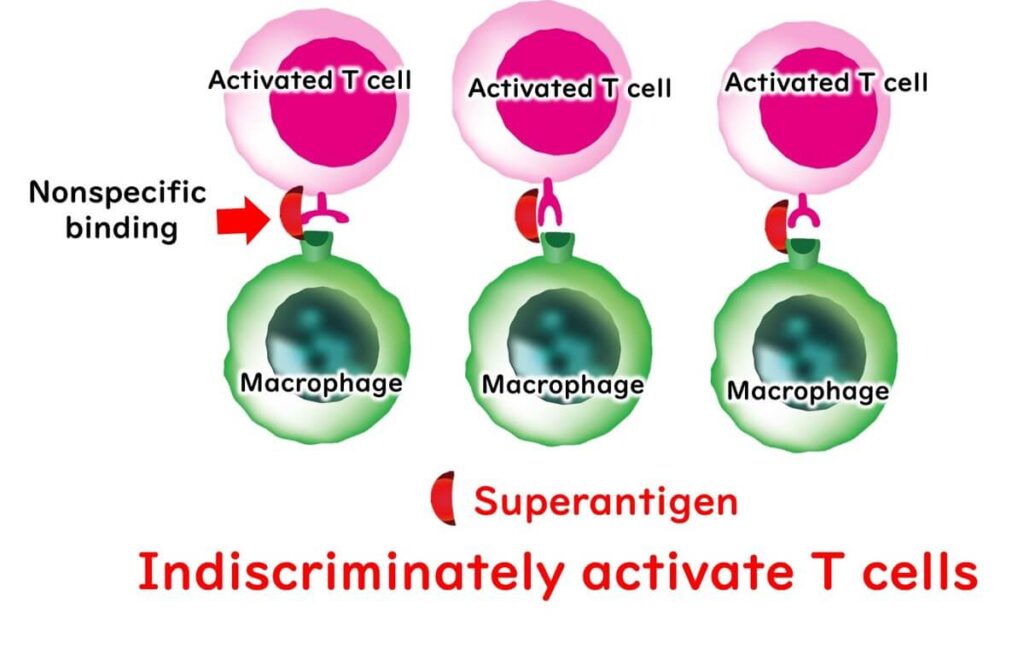
How Does This Overreaction Affect the Body?
Imagine a hacker triggering a nationwide police alarm system. Instead of targeting a specific threat, the system sends out random alerts, overwhelming law enforcement with false alarms. Similarly, the massive T-cell activation caused by superantigens results in a “cytokine storm” – an excessive immune response where cytokines (immune signaling molecules) damage healthy tissues and cause widespread inflammation.

This is precisely what happens when S. aureus enterotoxins act as superantigens, contributing to severe inflammation and tissue damage during skin infections.
Staphylococcus aureus – The Culprit Behind Toxin-Induced Food Poisoning
Beyond its role as a skin resident, Staphylococcus aureus is also a notorious contributor to foodborne illnesses, particularly due to its production of heat-stable enterotoxins. This section delves into the mechanisms behind its toxic effects and why food safety measures must focus on prevention.
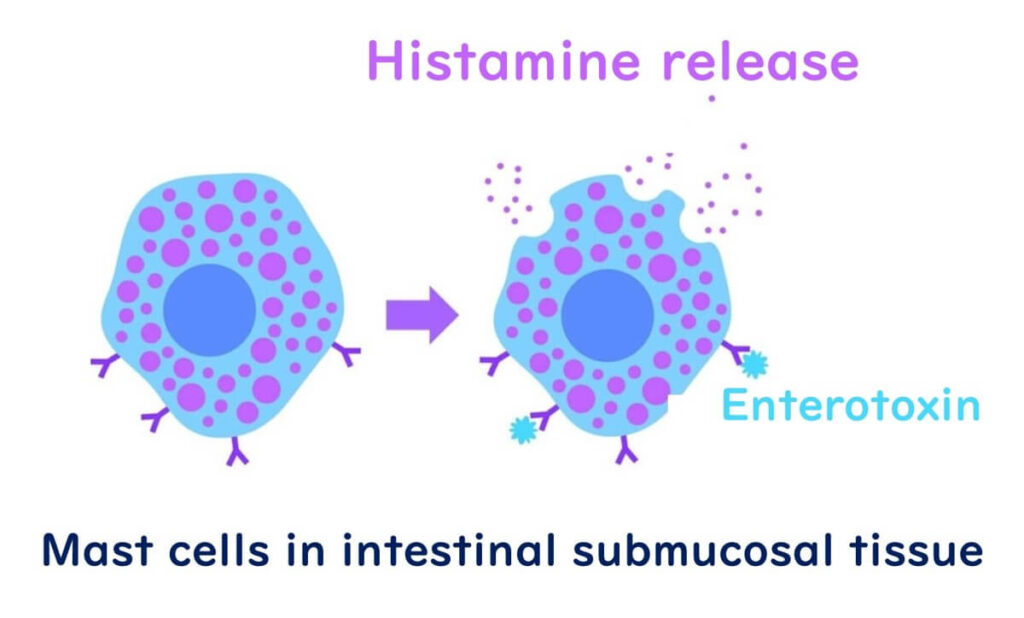
How Enterotoxin Triggers Vomiting
One of the hallmark symptoms of foodborne illness caused by S. aureus is vomiting, long attributed to its enterotoxins. However, the precise mechanism remained unclear until a 2019 study shed light on the process. Here’s what happens:
- Enterotoxin interacts with fat cells beneath the intestinal lining, stimulating the release of histamine.
- This histamine release activates nerve signals, which ultimately trigger the vomiting reflex.
Essentially, S. aureus enterotoxins hijack the body’s natural mechanisms, causing significant gastrointestinal distress.
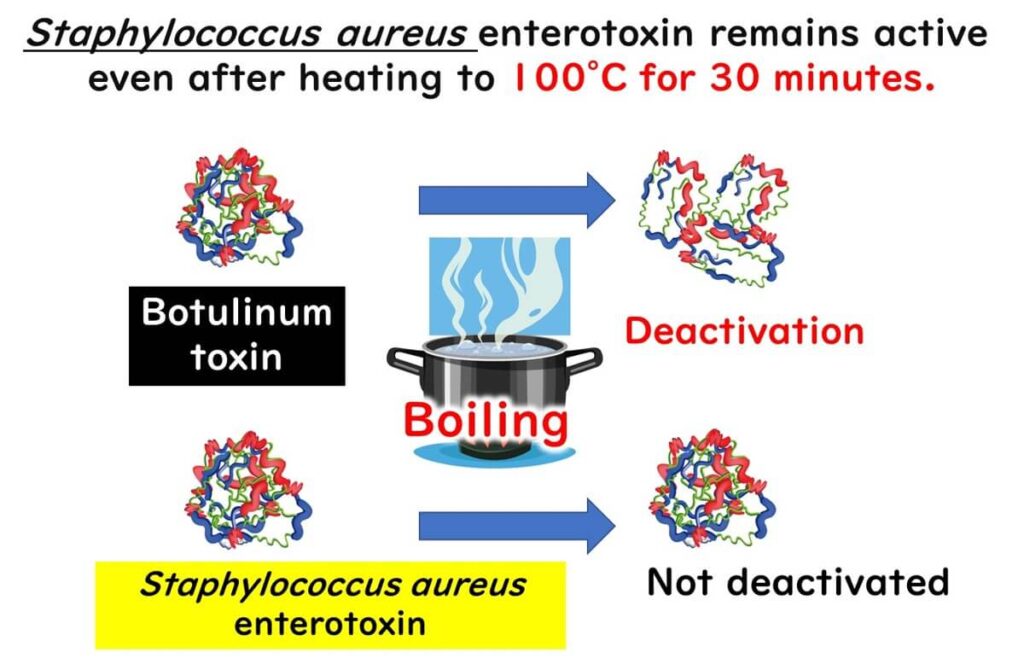
Enterotoxin: The Heat-Resistant Threat
A defining characteristic of S. aureus enterotoxins is their remarkable heat resistance. Unlike most bacteria and toxins that are destroyed during cooking, these enterotoxins remain active even after 30 minutes of boiling.
This resilience highlights the critical importance of food safety practices aimed at preventing S. aureus contamination in the first place, as cooking alone cannot neutralize its toxic effects. Preventative measures, such as proper handling, storage, and hygiene, are essential to mitigate the risk of foodborne illness.
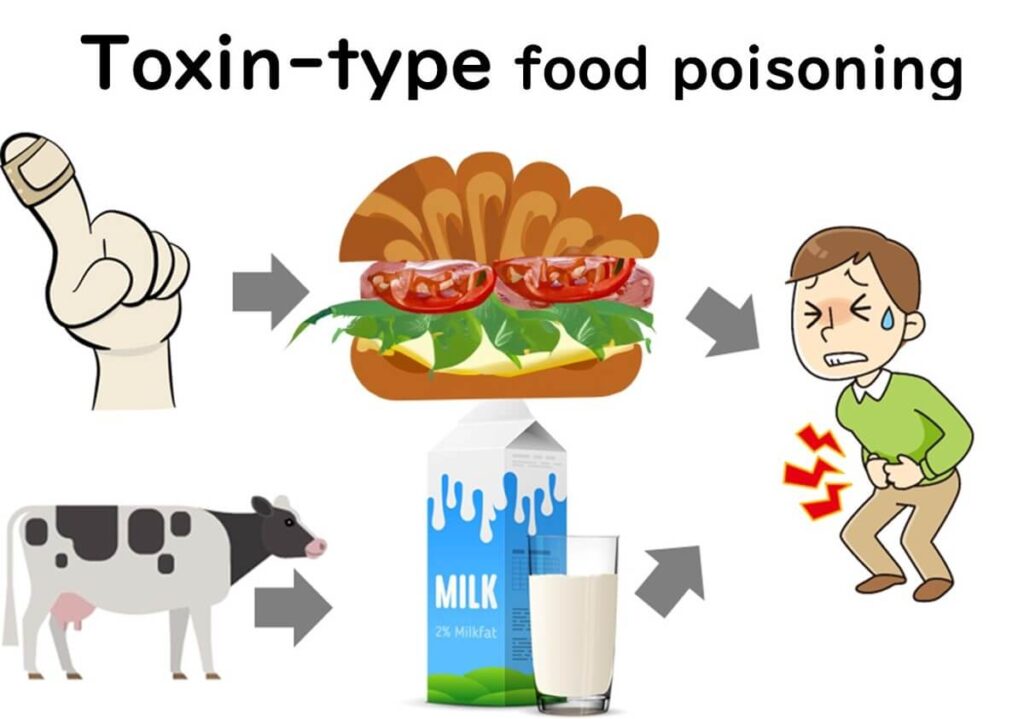
Foods Prone to Staph Food Poisoning
The largest outbreak of Staphylococcus aureus-related food poisoning occurred in Japan in 2000, affecting 14,849 people and hospitalizing 5,413. The cause? Contamination by enterotoxin A in low-fat milk. This incident highlights how S. aureus, often found on human skin and animal udders, can easily infiltrate food supplies.
Common foods susceptible to S. aureus contamination include:
- Dairy products (e.g., milk, cheese)
- Processed meats (e.g., ham, sausages)
- Prepared foods (e.g., salads, sandwiches)
- Bakery items (e.g., cream-filled pastries)
In Japan, traditional foods such as onigiri, bento side dishes, and lunch boxes are also frequent carriers. Contamination often occurs during food preparation when bacteria are transferred from the hands or noses of food handlers. Once on the food, S. aureus can multiply during storage or transportation, especially in warm conditions.
To mitigate the risk, preventing initial contamination is key. Ensuring proper hygiene and limiting direct human contact with food can significantly reduce outbreaks.
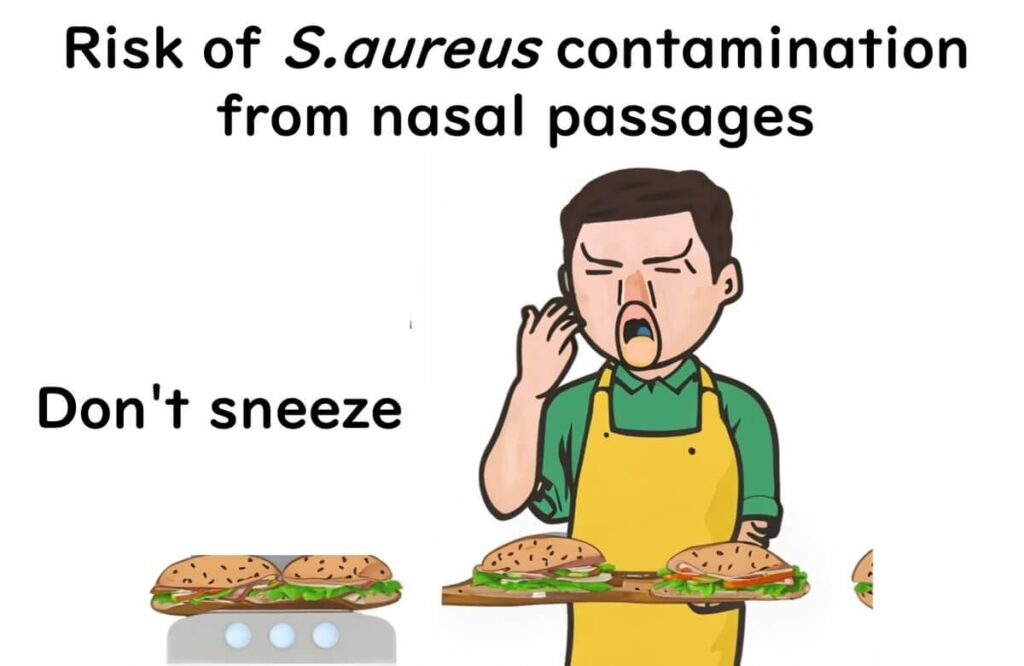
What Food Handlers Need to Be Wary Of
Preventing Staphylococcus aureus contamination requires more than avoiding bare-handed contact with food. These bacteria also reside in the nasal passages of humans, making sneezing a potential contamination source.
To minimize risks, food handlers should:
- Always wear gloves when handling food to avoid direct contact.
- Wear masks during food preparation to prevent bacteria from sneezes or nasal secretions contaminating food.
- Practice proper hand hygiene, including washing hands before and after handling food.
Wearing protective gear, such as gloves and masks, not only ensures a professional appearance but also serves as an effective barrier against bacterial transmission. These measures are vital for maintaining food safety and preventing S. aureus-related illnesses.
Staphylococcus aureus as a Marker in EU Process Hygiene Standards
In the European Union, food safety regulations emphasize not only the final product's quality but also the hygiene of the manufacturing process. Within these stringent guidelines, Staphylococcus aureus serves as a key indicator for process hygiene. Specifically, regulatory bodies focus on detecting the coagulase-positive type of S. aureus as part of their contamination monitoring efforts.
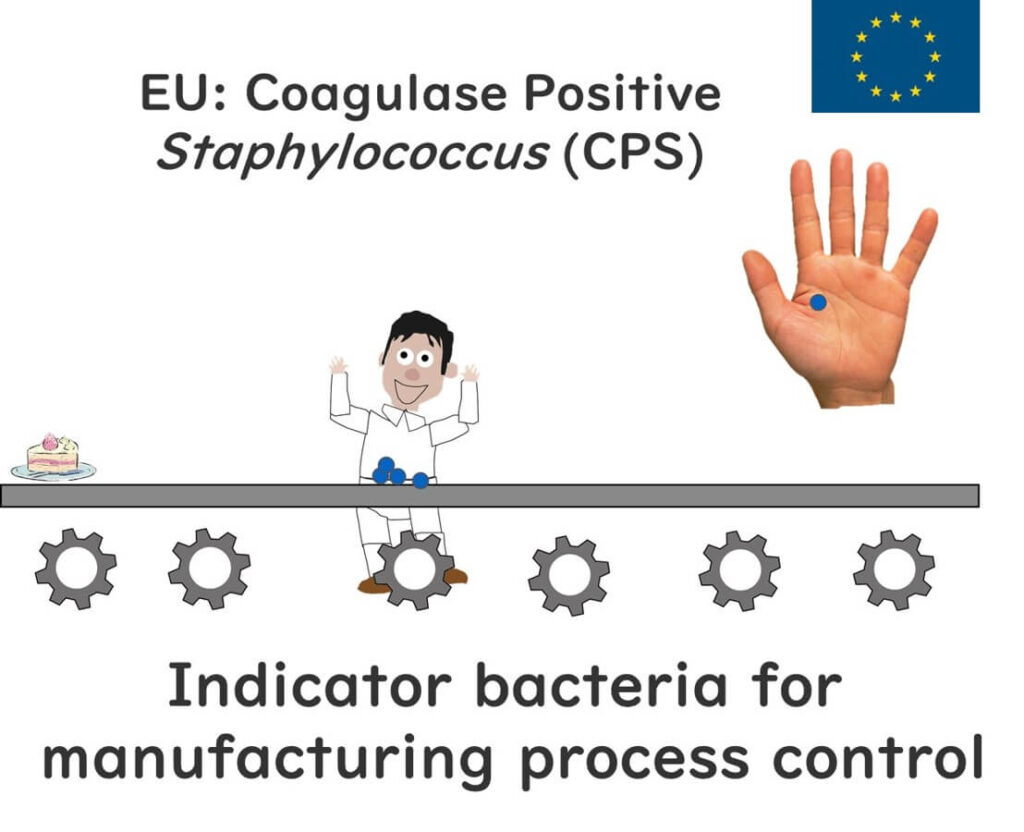
The Link Between Coagulase-Positive and Enterotoxin Production
Coagulase-positive Staphylococcus aureus is frequently used as a benchmark for food hygiene standards. However, it’s important to note that coagulase is primarily a virulence factor related to skin infections, where it enables S. aureus to evade the immune system. On the other hand, food poisoning is typically caused by enterotoxins produced by S. aureus, not by coagulase itself.
So why test for coagulase rather than directly identifying enterotoxin-producing bacteria? The answer lies in simplicity and efficiency. The coagulase test is quick and straightforward: mixing blood plasma with a sample to see if it clots. Testing for enterotoxins, in contrast, is far more complex, requiring specialized equipment and extended analysis times.
Fortunately, coagulase-positive strains of S. aureus are highly correlated with the production of enterotoxins. Thus, using the coagulase test offers a practical and reliable proxy for identifying toxin-producing strains, effectively addressing two concerns with one method.